Common Comorbidities in Comorbid Complex ADHD:
Prevalence, Age of Onset, Diagnosis, and Clinical Implications

Andrew J. Cutler, MD
Associate Clinical Professor
Department of Psychiatry
SUNY Upstate Medical University
Syracuse, New York
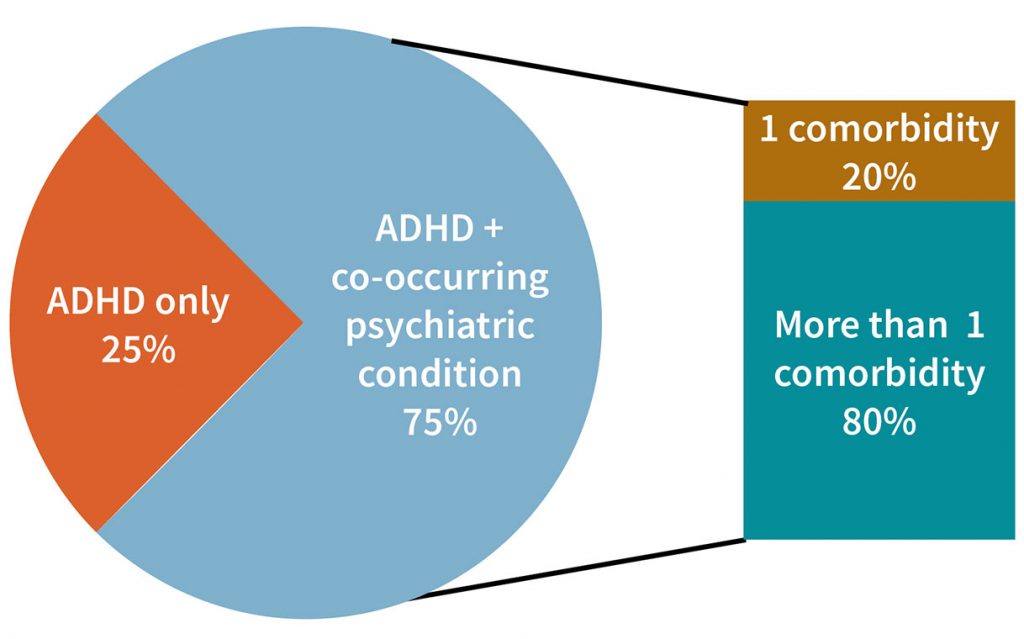
Majority of People With ADHD Have at Least One Comorbidity1
Potential Explanations for Comorbidities in ADHD2,3
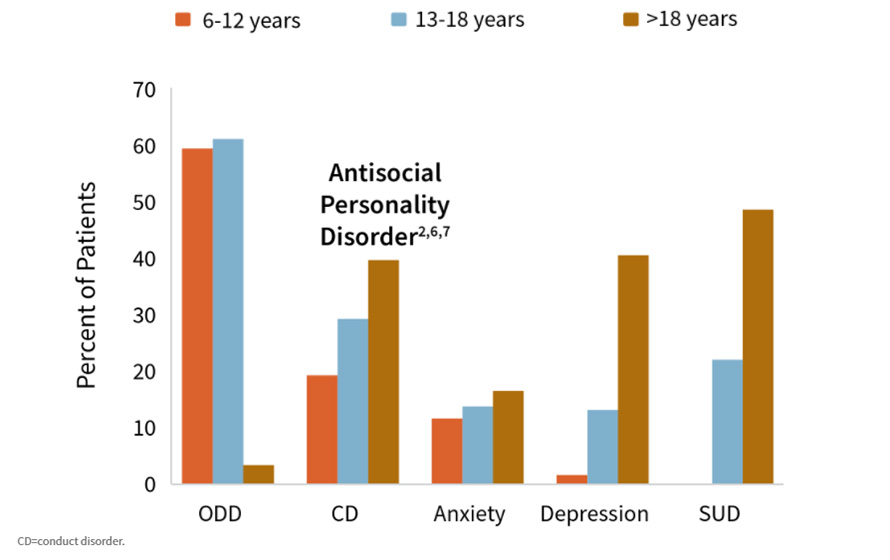
Comorbidity Profiles Change With Age2,4-7
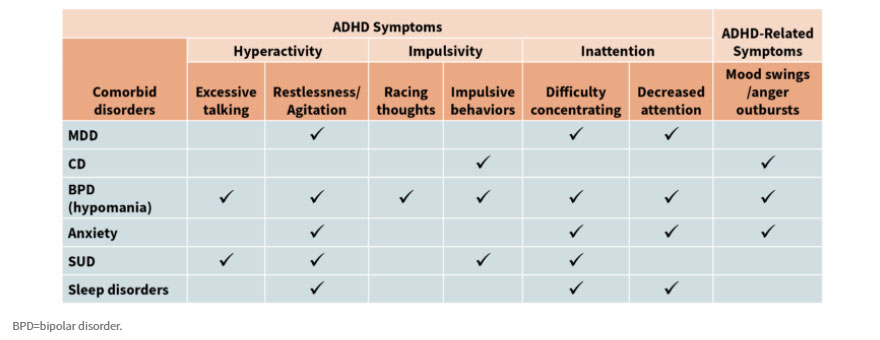
Overlapping Symptoms of ADHD and Comorbidities11
Diagnosing ADHD12

Differentiating Depression From ADHD2
To differentiate ADHD from depression, it is necessary to identify which symptoms of depression overlap with ADHD and which are distinct. Overlapping symptoms include loss of motivation, problems concentrating, and restlessness or irritability. If patients have any of these symptoms, it could be ADHD, depression, or both.2
Symptoms of depression that overlap with symptoms of ADHD
- Loss of motivation, demoralization
- Problems concentrating
- Being restless or irritable
Characteristics of depression that are distinct from ADHD
- Feeling sad or hopeless
- Feeling tired or "slowed down"
- Changes in eating and/or sleeping, neurovegetative symptoms
- Thoughts of death or suicide
- Episodic (while ADHD has a continuous course since childhood)
References
1. Banaschewski T, Becker K, Döpfner M, Holtmann M, Rösler M, Romanos M. Attention‑deficit/hyperactivity disorder. Dtsch Arztebl Int. 2017;114(9):149‑159.
2. CADDRA. Canadian ADHD Practice Guidelines. 4th ed. 2018. Available at: www.caddra.ca/wp-content/uploads/CADDRA-Guidelines-4th-Edition_-Feb2018.pdf. Accessed August 29, 2019.
3. Pliszka SR. Comorbidity of attention-deficit/hyperactivity disorder with psychiatric disorder: an overview. J Clin Psychiatry. 1998;59 Suppl 7:50‑58.
4. Turgay A, Ansari R. Major depression with ADHD: in children and adolescents. Psychiatry (Edgmont). 2006;3(4):20‑32.
5. Kollins SH. ADHD, substance use disorders, and psychostimulant treatment: current literature and treatment guidelines. J Atten Disord. 2008;12(2):115‑125.
6. Biederman J, Petty CR, Woodworth KY, Lomedico A, Hyder LL, Faraone SV. Adult outcome of attention-deficit/hyperactivity disorder: a controlled 16‑year follow‑up study. J Clin Psychiatry. 2012;73(7):941‑950.
7. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington D.C.: 2013.
8. Goodman DW. ADHD in adults: update for clinicians on diagnosis and assessment. Prim Psychiatry. 2009;16(11):21‑30.
9. Faraone SV, Asherson P, Banaschewski T, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers. 2015;1:15020.
10. Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90 Suppl 1:i2‑i7.
11. Kooij JJ, Huss M, Asherson P, et al. Distinguishing comorbidity and successful management of adult ADHD. J Atten Disord. 2012;16(5 Suppl):3S‑19S.
12. American Academy of Pediatrics. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007‑1022.